Stroke Pathway Coordination (Thrombolysis Referral)
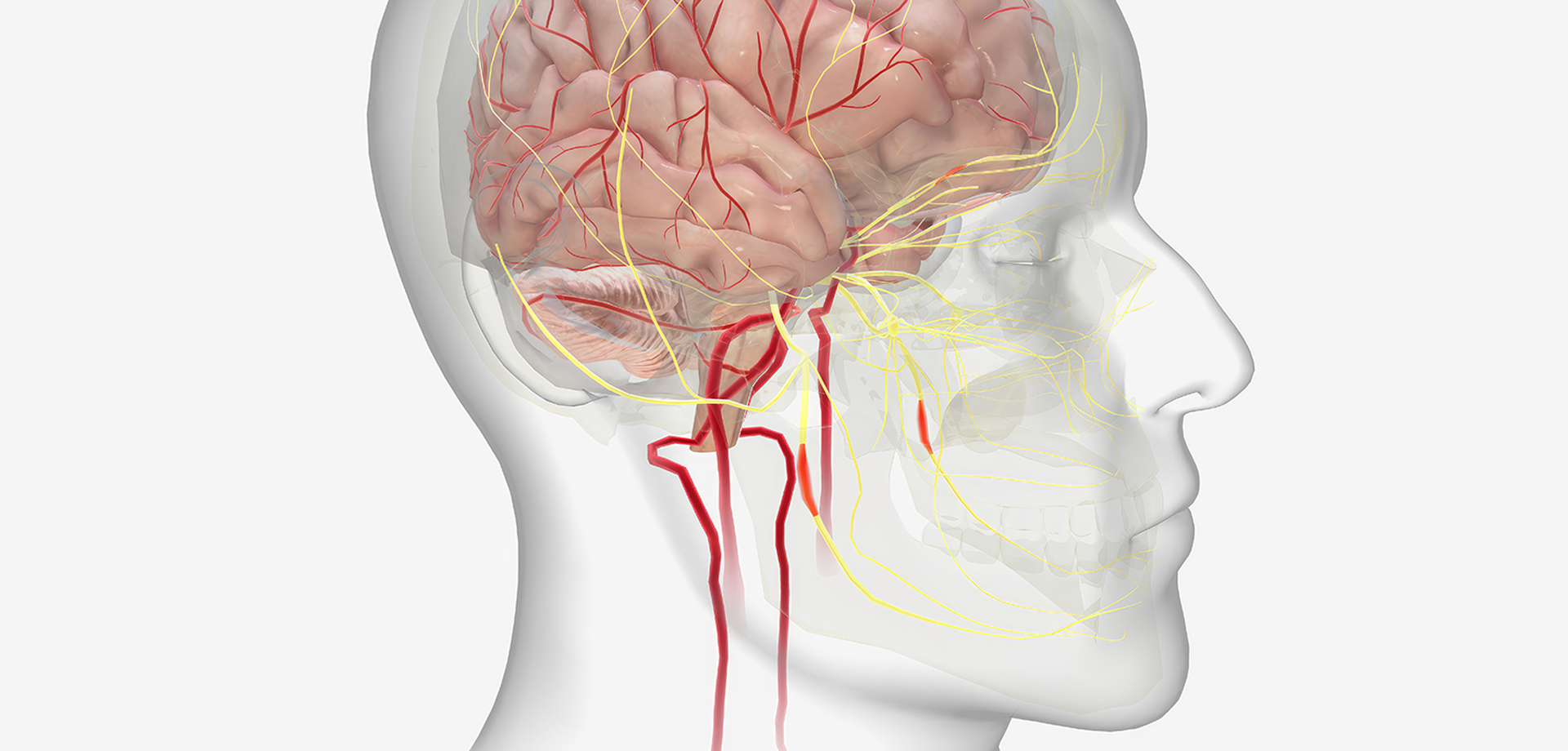
Stroke pathway coordination is a time-sensitive neurological service designed to ensure rapid diagnosis and immediate intervention for acute stroke patients. In Dubai and across the UAE, structured “Code Stroke” systems allow seamless activation of emergency imaging, neurologist evaluation, and thrombolysis referral when indicated. Time is critical in stroke management, as every minute of delay results in irreversible brain cell damage.
When a patient presents with sudden weakness, facial drooping, speech difficulty, vision changes, or imbalance, immediate neurological assessment is initiated. Brain imaging, typically an urgent CT scan, distinguishes ischemic stroke from hemorrhagic stroke. Only ischemic strokes may qualify for thrombolytic therapy within the recommended therapeutic window.
Neurologists evaluate eligibility for intravenous thrombolysis based on symptom onset timing, imaging findings, medical history, and contraindications. Early administration of clot-dissolving medication restores blood flow to affected brain areas and significantly improves recovery outcomes.
For large vessel occlusions, referral for mechanical thrombectomy at specialized centers may be arranged. Coordinated communication between emergency physicians, neurologists, radiologists, and interventional teams ensures rapid escalation of care.
Post-acute stroke management includes risk factor evaluation, blood pressure control, anticoagulation when appropriate, and rehabilitation referral. Secondary prevention strategies are implemented to reduce recurrence risk.
In the UAE, increasing public awareness of stroke symptoms through FAST (Face, Arm, Speech, Time) campaigns supports early hospital presentation. Structured stroke pathways reduce treatment delays and improve functional outcomes.
Stroke coordination extends beyond acute intervention. Long-term neurologic follow-up monitors recovery, cognitive changes, and motor function. Multidisciplinary rehabilitation supports functional independence.
Stroke pathway coordination represents a life-saving neurological service. Through rapid diagnosis, thrombolysis referral, and comprehensive follow-up, neuroscience teams significantly improve survival and recovery rates.
When a patient presents with sudden weakness, facial drooping, speech difficulty, vision changes, or imbalance, immediate neurological assessment is initiated. Brain imaging, typically an urgent CT scan, distinguishes ischemic stroke from hemorrhagic stroke. Only ischemic strokes may qualify for thrombolytic therapy within the recommended therapeutic window.
Neurologists evaluate eligibility for intravenous thrombolysis based on symptom onset timing, imaging findings, medical history, and contraindications. Early administration of clot-dissolving medication restores blood flow to affected brain areas and significantly improves recovery outcomes.
For large vessel occlusions, referral for mechanical thrombectomy at specialized centers may be arranged. Coordinated communication between emergency physicians, neurologists, radiologists, and interventional teams ensures rapid escalation of care.
Post-acute stroke management includes risk factor evaluation, blood pressure control, anticoagulation when appropriate, and rehabilitation referral. Secondary prevention strategies are implemented to reduce recurrence risk.
In the UAE, increasing public awareness of stroke symptoms through FAST (Face, Arm, Speech, Time) campaigns supports early hospital presentation. Structured stroke pathways reduce treatment delays and improve functional outcomes.
Stroke coordination extends beyond acute intervention. Long-term neurologic follow-up monitors recovery, cognitive changes, and motor function. Multidisciplinary rehabilitation supports functional independence.
Stroke pathway coordination represents a life-saving neurological service. Through rapid diagnosis, thrombolysis referral, and comprehensive follow-up, neuroscience teams significantly improve survival and recovery rates.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7



 04 406 3000
04 406 3000  04 406 3000
04 406 3000







