Parenteral Nutrition Coordination
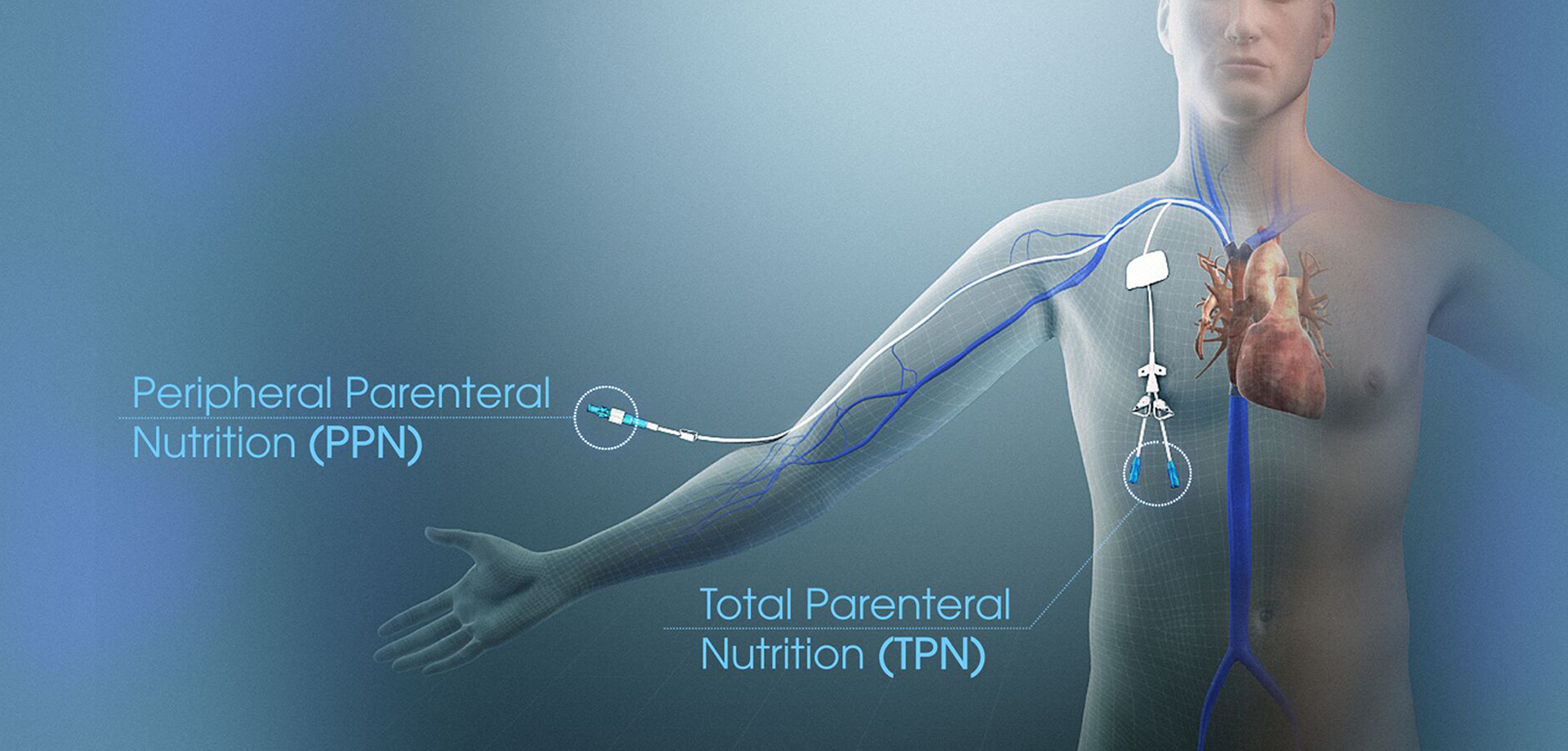
Parenteral nutrition coordination is a highly specialized clinical service for patients who cannot meet their nutritional requirements through the gastrointestinal tract due to severe illness, bowel dysfunction, or critical medical conditions. Parenteral nutrition provides nutrients directly into the bloodstream, bypassing the digestive system, and requires meticulous planning, monitoring, and interdisciplinary coordination to ensure safety and effectiveness.
Parenteral nutrition is indicated in conditions such as intestinal failure, severe malabsorption, prolonged ileus, bowel obstruction, high-output fistulas, and certain critical care scenarios. Coordination begins with a detailed clinical and nutritional assessment to determine indication, duration, and risk profile. Decisions consider metabolic demands, organ function, infection risk, and vascular access.
The formulation of parenteral nutrition is highly individualized. Macronutrients, micronutrients, fluids, and electrolytes are calculated based on body weight, clinical condition, laboratory values, and metabolic response. Coordination with pharmacy services ensures accurate compounding, stability, and compatibility of nutrient solutions.
Monitoring is intensive and ongoing. Laboratory values, fluid balance, liver function, glucose control, and electrolyte levels are closely tracked to prevent complications such as infections, metabolic disturbances, and organ dysfunction. Adjustments are made promptly in response to clinical and biochemical changes.
Education and communication are essential, particularly for patients requiring long-term or home parenteral nutrition. Caregivers are trained in catheter care, infusion techniques, and complication recognition. A structured coordination model minimizes risk and supports continuity of care.
Parenteral nutrition coordination is a life-sustaining intervention when managed appropriately. Through expert oversight and multidisciplinary collaboration, it supports recovery, prevents severe malnutrition, and improves survival in complex clinical scenarios.
Parenteral nutrition is indicated in conditions such as intestinal failure, severe malabsorption, prolonged ileus, bowel obstruction, high-output fistulas, and certain critical care scenarios. Coordination begins with a detailed clinical and nutritional assessment to determine indication, duration, and risk profile. Decisions consider metabolic demands, organ function, infection risk, and vascular access.
The formulation of parenteral nutrition is highly individualized. Macronutrients, micronutrients, fluids, and electrolytes are calculated based on body weight, clinical condition, laboratory values, and metabolic response. Coordination with pharmacy services ensures accurate compounding, stability, and compatibility of nutrient solutions.
Monitoring is intensive and ongoing. Laboratory values, fluid balance, liver function, glucose control, and electrolyte levels are closely tracked to prevent complications such as infections, metabolic disturbances, and organ dysfunction. Adjustments are made promptly in response to clinical and biochemical changes.
Education and communication are essential, particularly for patients requiring long-term or home parenteral nutrition. Caregivers are trained in catheter care, infusion techniques, and complication recognition. A structured coordination model minimizes risk and supports continuity of care.
Parenteral nutrition coordination is a life-sustaining intervention when managed appropriately. Through expert oversight and multidisciplinary collaboration, it supports recovery, prevents severe malnutrition, and improves survival in complex clinical scenarios.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7



 04 406 3000
04 406 3000  04 406 3000
04 406 3000







