Craniotomy for Tumor
Craniotomy for tumor removal is one of the most critical and sophisticated procedures in modern neurosurgery, performed to access and treat abnormal growths within the brain. In the UAE, where advanced neuroscience infrastructure continues to evolve rapidly, craniotomy procedures are conducted within highly specialized operating suites equipped with intraoperative imaging, neuro-navigation systems, and advanced monitoring technologies designed to enhance surgical precision and safety. A craniotomy involves temporarily removing a section of the skull to allow direct access to the brain, enabling neurosurgeons to remove tumors, relieve pressure, obtain biopsies, or address associated complications while preserving vital neurological structures.
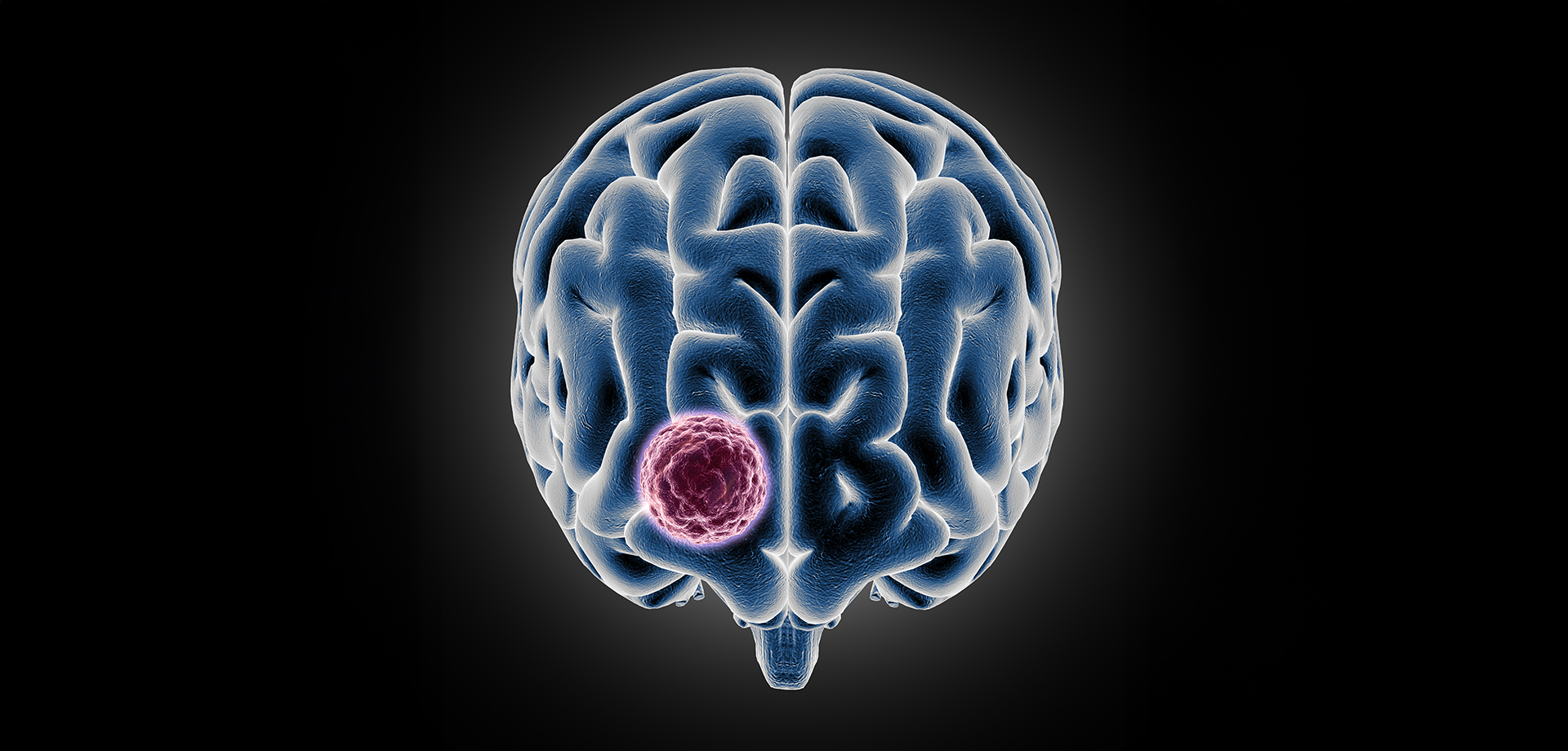
Brain tumors may be primary, originating within brain tissue, or secondary, spreading from other parts of the body. Symptoms can vary depending on tumor location and size and may include persistent headaches, seizures, weakness, speech difficulties, personality changes, or visual disturbances. Imaging studies such as MRI and CT scans play a crucial role in surgical planning, allowing the neurosurgical team to map the tumor’s relationship to functional brain areas. In UAE neuroscience centers, multidisciplinary tumor boards frequently review cases to determine optimal timing and surgical strategy, aligning neurosurgery with oncology, radiology, and rehabilitation services.
During craniotomy for tumor removal, precision is paramount. The goal is maximal safe resection, meaning the surgeon aims to remove as much of the tumor as possible while preserving neurological function. Modern operating microscopes, cortical mapping technologies, and real-time monitoring systems enhance the ability to differentiate tumor tissue from normal brain tissue. In selected cases, minimally invasive approaches may be incorporated to reduce tissue disruption. After tumor removal, the bone flap is carefully repositioned and secured, and patients are monitored in specialized neurocritical care units.
Post-operative care is equally vital and often includes neurological monitoring, imaging to confirm tumor resection, and structured rehabilitation when required. In the UAE, integrated neuroscience programs emphasize early mobilization, cognitive assessment, and physiotherapy planning to support functional recovery. For malignant tumors, coordination with oncology teams ensures continuity of care through adjunctive therapies where appropriate. Emotional and psychological support is also emphasized, recognizing that brain tumor surgery affects patients and families profoundly.
Craniotomy for tumor remains a cornerstone of brain tumor management, particularly when tumors cause mass effect, neurological deficits, or increased intracranial pressure. Advances in neuro-navigation and intraoperative imaging have significantly improved outcomes compared to historical approaches, reducing complication rates and improving recovery timelines. In Dubai and across the UAE, neurosurgical centers position themselves as regional hubs for complex brain surgery, offering internationally benchmarked standards, advanced technology, and multidisciplinary expertise.
The decision to proceed with craniotomy is based on tumor characteristics, patient health status, neurological findings, and overall treatment goals. Transparent communication, detailed preoperative assessment, and structured follow-up planning define high-quality neurosurgical care in the region. With increasing awareness and early detection through advanced imaging, more patients are being evaluated at earlier stages, improving long-term neurological outcomes.
Brain tumors may be primary, originating within brain tissue, or secondary, spreading from other parts of the body. Symptoms can vary depending on tumor location and size and may include persistent headaches, seizures, weakness, speech difficulties, personality changes, or visual disturbances. Imaging studies such as MRI and CT scans play a crucial role in surgical planning, allowing the neurosurgical team to map the tumor’s relationship to functional brain areas. In UAE neuroscience centers, multidisciplinary tumor boards frequently review cases to determine optimal timing and surgical strategy, aligning neurosurgery with oncology, radiology, and rehabilitation services.
During craniotomy for tumor removal, precision is paramount. The goal is maximal safe resection, meaning the surgeon aims to remove as much of the tumor as possible while preserving neurological function. Modern operating microscopes, cortical mapping technologies, and real-time monitoring systems enhance the ability to differentiate tumor tissue from normal brain tissue. In selected cases, minimally invasive approaches may be incorporated to reduce tissue disruption. After tumor removal, the bone flap is carefully repositioned and secured, and patients are monitored in specialized neurocritical care units.
Post-operative care is equally vital and often includes neurological monitoring, imaging to confirm tumor resection, and structured rehabilitation when required. In the UAE, integrated neuroscience programs emphasize early mobilization, cognitive assessment, and physiotherapy planning to support functional recovery. For malignant tumors, coordination with oncology teams ensures continuity of care through adjunctive therapies where appropriate. Emotional and psychological support is also emphasized, recognizing that brain tumor surgery affects patients and families profoundly.
Craniotomy for tumor remains a cornerstone of brain tumor management, particularly when tumors cause mass effect, neurological deficits, or increased intracranial pressure. Advances in neuro-navigation and intraoperative imaging have significantly improved outcomes compared to historical approaches, reducing complication rates and improving recovery timelines. In Dubai and across the UAE, neurosurgical centers position themselves as regional hubs for complex brain surgery, offering internationally benchmarked standards, advanced technology, and multidisciplinary expertise.
The decision to proceed with craniotomy is based on tumor characteristics, patient health status, neurological findings, and overall treatment goals. Transparent communication, detailed preoperative assessment, and structured follow-up planning define high-quality neurosurgical care in the region. With increasing awareness and early detection through advanced imaging, more patients are being evaluated at earlier stages, improving long-term neurological outcomes.
Quick Contact
If you have any questions simply use the following contact details.

Working Hours
-
Out-patient Department
Monday to Saturday 08:00 AM - 09:00 PM
Sunday 10:00 AM - 06:00 PM
-
Emergency Department & Pharmacy
Sunday to Saturday 24x7



 04 406 3000
04 406 3000  04 406 3000
04 406 3000







