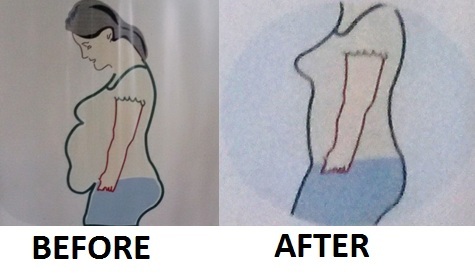
Hanging abdomen with an apron is unsightly and uncomfortable for any woman. Not able to wear the dress of their choice is so depressing to anyone. The self esteem gets down with every morning seeing the self profile. But they can be happy that there is a sure way out.
Causes of hanging abdomen
1) Overweight or obesity : General adiposity (excess fat) as part of increase in Body Mass Index can cause an increase in abdominal circumference. The ideal BMI is 18-23. Once it is above 23 till 27.5 it is overweight and 27.5 onwards is obesity. BMI is calculated as weight in Kg/Ht in M2 e.g. If a person has 100kg weight and 2m height, BMI= 100kg/ 2m x 2m=25 Kg/M2
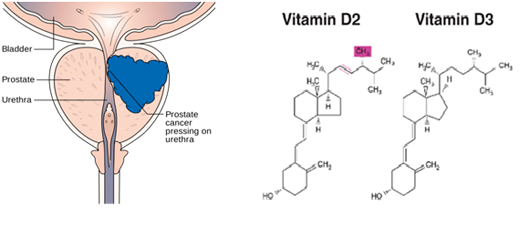
2) Truncal Obesity (Abdominal obesity) : Increasing abdominal obesity is more dangerous than the overall increase in weight. Ideally, the abdominal circumference at umbilical level should be below 80 cm in women. The increase in BMI and abdominal circumference leads to various medical illness like Diabetes, hypertension (increase in blood pressure), dyslipedemia (increase in cholesterol), sleep apnoea (breathing difficulty/ snoring with respiratory arrest), PCOS (Polycystic ovarian disease) and fatty liver. It also increase the risk of cancers of breast and ovary.
3) Divarication Recti (separation of muscles of abdominal wall) : This happens mainly and commonly following pregnancy when there is excessive stretch of abdominal wall muscles making it fall apart from the midline. This leads to bulging of abdomen and patient will have a state similar to pregnancy look. This is highly distressing to any woman. The abdominal bulge will be such that it projects out and comes anterior than breast level in a profile view.
4) Ventral hernia : muscle defect with herniation/ projection of abdominal contents in to the sac formed at the muscle weakness. The intestines or omentum get trapped in this defect and can cause life threatening problems.
5) Sagging fat and skin : The lower abdominal wall fat and skin is redundant (extra) and hangs down in an unsightly manner. The skin sagging may be unrelated to the muscle weakness. The pulling down of the abdominal wall by the weight of this apron itself will be causing discomfort and muscle weakness. The disfigurement in these patients is unexplainable.
Assessment
Patients need to consult a surgeon who is well-versed with the problem and its corrective measures. Detailed physical examination with abdominal girth, height, weight, BMI, BP, Pulse, oxygen saturation to be checked. The co-existing problems like diabetes, hypertension, snoring, respiratory difficulty with walking, menstrual irregularities, stress incontinence and psychological problem (mainly depression).
The psychological impact of these illness on the patient is very significant. They will be always worried about and other is depression seeing the bad body contour every day. Being not able to wear the dress they like and not able to move around comfortably also keeps them introverts and less sociable. Many jobs also demand people with normal BMI and body shapes. Even promotions are jeopardized by these abnormalities. The associated medical problems and the need for medication for the same will also be making patients uncomfortable and dissatisfied in life.
Treatment Options
Those who have increased BMI should be advised for weight reduction. To a good extend it is possible by diet regulations and exercise. There are some drugs available to reduce weight but it helps in reducing weight around 4-5 kg only. Those with higher BMI will be benefitted by intra-gastric balloon placement or by bariatric surgery of which sleeve gastrectomy is the best. Abdominal obesity also gets controlled to a great extent by these procedures.
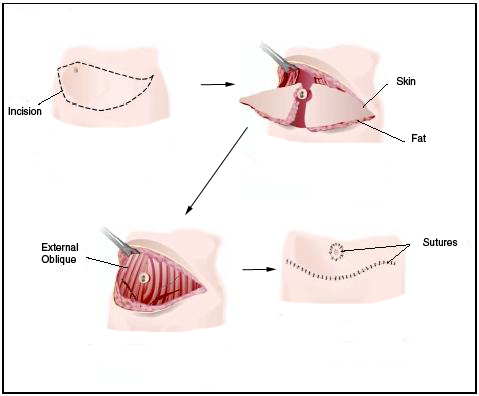
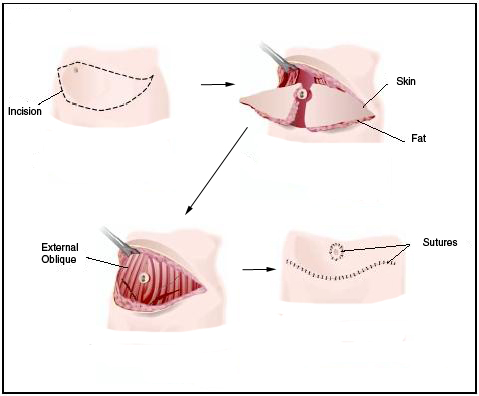
Divarication of recti (the separation of muscle in the central abdomen), the ventral hernia and sagging skin with fat (the abdominal apron) needs tummy tuck (abdominoplasty). The exercises to tone the abdominal wall, weight reduction or application of any kind of solutions or application of slim devices like vibrators are not going to give any kind of benefit to these patients.
The procedure of tummy tuck involves a pre-hospitalization checkup including blood tests. Ultrasound abdomen is performed to rule out any other surgical problem in abdomen like an ovarian cyst or gall bladder stones which can be talked at the same time. The necessary consultations will also be done with other specialists as needed.
The operation is done under anaesthesia, either general or regional, so that patient will be comfortable. The incision will be made at the lowest skin crease of abdomen to give excellent cosmetic outcome. The skin and subcutaneous fat will be mobilized. The muscles which are far apart will be brought together. In case of hernia a net like material (mesh) will be used to give additional strength. The excess fat and skin will be removed and wound closed. The wound closure is also done in a careful manner with no stitches outside. This also will add to the perfect healing with very minimal scar. The scar will be completely hidden by the smallest of dress.
Patient needs to be in hospital for 2-3 days and can resume normal activities after that. All kinds of job can be started within two weeks time. Wearing an abdominal binder during this period will give additional comfort.
The outcomes are such great that patients get immediate results and regain self esteem. The profile changes and any modern dress will suit the person. The medical issues related to the divarication like dragging pain in abdomen and backache due to the abnormal posture and weight of ventral hernia will also get resolved. In those with higher BMI and sagging abdomen the procedure to reduce weight (sleeve gastrectomy) is done along with the tummy tuck thereby avoiding scars of the bariatric surgery and unnecessary second hospitalization. Combination of these procedures is an innovative method developed at our centre to give maximal benefit for patient with superior quality of life.
Feedback:
Dear Dr Padmakumar
My tummy tuck (abdominoplasty) was done in september 2013. I was very uncomfortable and had very strong inferiority complex due to my sagging abdomen and hernia. My friends are asking me ” oh you are pregnant again”. After my tummy tuck surgery , ” I can’t believe , all tummy had gone and I was flying in heights”.
Now am happy that I can wear any kind of dress I wish and my confidence level increased.
Thank you all doctors “you are all so special in my life”
Mrs. Liji Chandran
Dr. R. Padmakumar MBBS, DNB, MNAMS, DipALS, FAIS
Specialist Surgeon , International Modern Hospital, Dubai
Senior Consultant Surgeon & Medical Director, Sunrise Hospital, Cochin (Specialist in Laparoscopy, Hernia, Cancer, Endoscopic Thyroid Surgery,
Thoracoscopy, Obesity and Diabetic Surgery)
GC Member – Association of Surgeons of India
National President Elect – Indian Hernia Society
Jt. Secretary – Indian Association of Endocrine Surgeons
Founder Member – Obesity and Metabolic Surgery Society of India &
Association of Minimal Access Surgeons of India
International Faculty of IASGO on Hernia and Diabetic Surgery
International Faculty of IFSO on Ileal Interposition (Diabetic Surgery)
Mob : +919447230370 (India) ; 00971567581025 (UAE)
Email : drrpadmakumar@gmail.com
Websites:
www.drrpadmakumar.com
www.diabetescuresurgery.com
www.obesitysurgeonkerala.com
www.endoscopythyroid.com


 It is important for these people to see a Surgeon at the earliest to enable an accurate diagnosis and initiate early treatment to prevent further complications. Over the counter medications and creams are of limited use as almost all of these conditions present with more or less the same complaints, however the treatment is completely different for each one of them.
It is important for these people to see a Surgeon at the earliest to enable an accurate diagnosis and initiate early treatment to prevent further complications. Over the counter medications and creams are of limited use as almost all of these conditions present with more or less the same complaints, however the treatment is completely different for each one of them. These however, need to be performed by experienced Surgeons who have undergone extensive training in this specialty and have the know how and technical expertise.
These however, need to be performed by experienced Surgeons who have undergone extensive training in this specialty and have the know how and technical expertise.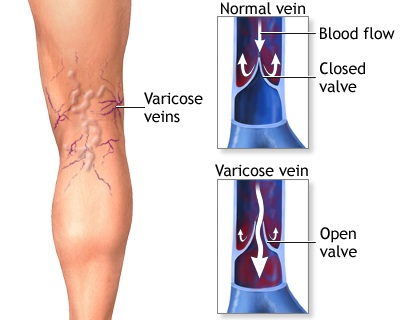
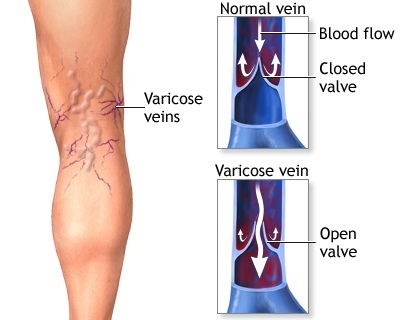 Varicose veins are swollen, twisted, and enlarged veins that you can see under the skin. They are often red or blue in color. They usually appear in the legs, but can occur in other parts of the body.
Varicose veins are swollen, twisted, and enlarged veins that you can see under the skin. They are often red or blue in color. They usually appear in the legs, but can occur in other parts of the body.