For as long as humans have lived, there has been the need to treat ailments — including spine issues. Thus, traditional methods of treating spinal issues have existed for thousands of years, even before the first-ever recorded operative spine surgery credited to Paul of Aegina in the 7th century.
However, minimally invasive spine surgery (MISS) is still a relatively new method of treatment. It started becoming popular in the 1990s due to advancements in medical technology.
This piece will be looking at what minimally invasive spine surgery (MISS) is, its benefits, types, and how to prepare if you’re to undergo surgery.
What is Minimally Invasive Spine Surgery (MISS)
Minimally invasive spine surgery (MISS) is a surgical procedure performed to treat or correct spinal problems. Some of the most common spinal issues treated using MISS are scoliosis, herniated disc, spinal stenosis, degenerative disc disease, etc.
The difference between MISS and the traditional open surgical method is that only small incisions are required to treat the patient with MISS.
Thus, here are the five major advantages of MISS.
Benefits of Minimally Invasive Spine Surgery (MISS)
Little Scars: Because Miss requires minimal incisions, patients get only small scarring and lesser risk of muscle damage.
Fast recovery: Due to minimal scarring, MISS’s healing process is faster compared to traditional methods.
Reduced infection risk: The risk of infection is drastically reduced because MISS involves little muscle and tissue tearing.
Minimal time at the hospital: Unlike regular spine surgeries, with minimally invasive spine surgery, you can go home within a few hours to 2 days after the surgery.
Types of Minimally Invasive Spine Surgery (MISS)
Spinal fusion: Using minimally invasive spine surgery, spinal fusion; that is, the joining of two or more bones in the spine, can be done to stop movement between the bones. This is usually required to treat spinal ailments like degenerative disc disease, fracture, scoliosis, etc. The benefit of using MISS for this type of surgery is that it improves recovery and reduces the chances of infection.
Lumbar disc arthroplasty: This procedure is an alternative to the more popular spinal fusion surgery. It involves replacing a degenerated disk in the lower part of the spine. In this case, an artificial disk made of cobalt-chromium and plastic is used to replace the worn-out disk.
Lumbar disc arthroplasty is a major surgery that involves dissecting muscles and tissues at the back. However, only a small incision is made between the lower abdominal muscles to get to the spine using the minimally invasive spine surgery method. Besides, MISS patients usually spend less time in the hospital post-operation.
Corpectomy: This procedure is usually employed to relieve pressure caused by a spinal tumor, fracture, bone spur, stenosis, etc. It involves the surgical removal of a bone or parts of it in the neck, mid-back, or lower back.
Discectomy: This involves the surgical removal of materials pressing against the spinal cord or nerve root. Discectomy is usually employed in treating medical issues like bone spur, nerve root compression, sciatica, etc.
Foraminotomy: As the name suggests, this procedure is employed to treat issues related to the foramen. That is the tunnel in the back where nerve roots exit the spinal cord. Usually, foraminotomy is done to widen the foramen to relieve the pains and muscle weakness caused by nerve root compression. Other conditions treated with this procedure include herniated disc, bone spur, foraminal stenosis, etc.
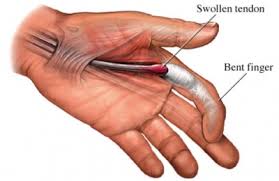
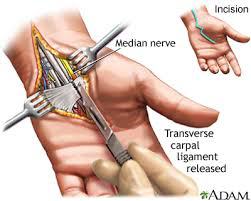
Laminectomy: Laminectomy involves the surgical removal of the lamina, the backbone protecting the spinal canal. This procedure is employed when there is a need to relieve spinal cord pains caused by spinal stenosis, bone spur, or herniated disc. By using minimally invasive spine surgery, this procedure can be completed within a few hours. The patients can also go home the same day.
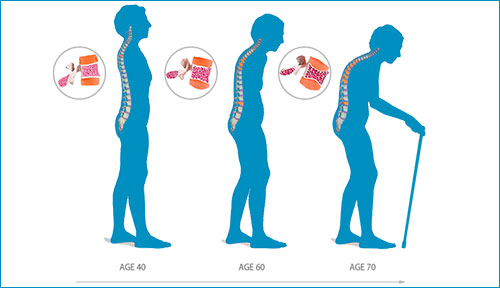
Kyphoplasty: This procedure is employed to restore a fractured vertebra to its original shape. This procedure is usually necessary when there is a compression fracture in the spine. Cancer, injuries, or osteoporosis; the thinning of the bones can cause such issues.
Spinal instrumentation: Spinal instrumentation is employed in minimally invasive spine surgeries to prevent movement in specific segments of the spine. It’s usually done after the surgery to ensure proper fusion and quicker healing post-operation.
Spinal Disorders Treated Using the MISS Method
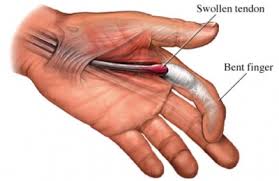
Herniated discs: This is one of the causes of back pains experienced by adults. Herniated discs occur when some of the inner core of an intervertebral disc breaks through its protective outer layer. This often causes back pain and inflammation of nerves surrounding the disc.
Scoliosis: It’s mostly common among children, but adults can also develop the condition. Scoliosis is an abnormal sideward curvature that may lead to uneven shoulders, hips, or waist. Mild scoliosis may require regular monitoring but no surgery. However, if the condition worsens, an orthopedic doctor can employ MISS to prevent permanent deformity.
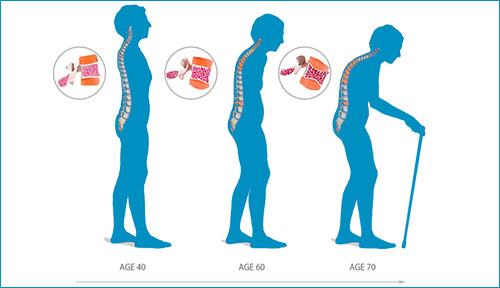
Degenerative disc disease: This disease occurs when the intervertebral discs stiffen and lose strength and shape. When this happens, the discs also lose the flexibility to absorb and distribute forces with spinal movements. Degenerative disc disease (DDD) is common in older adults. If left untreated, it could increase the chances of herniated discs.
Spinal stenosis: This occurs when the spaces within the spine are compressed or narrowed. This condition can cause numbness, muscle weakness, pain, tingling sensation at the back and neck, and sometimes in the arms and legs. In some cases, there are mild to no symptoms. In severe cases, spinal surgery may be required to create more openings for the spinal cord.
How To Know If You Need a Minimally Invasive Spine Surgery
It’s important to note that not every back pain requires MISS or any other kind of surgery.
If you are experiencing minor back pains, it may be because of your sitting posture, lack of sleep and exercise, etc. So firstly, try to correct such habits.
That said, it’s essential to seek medical attention immediately if you are experiencing continuous pains or irritation in your neck and back areas.
How to prepare for a MISS surgery?
Ideally, once your orthopedic doctor confirms that you need to undergo a MISS or any spine surgery, he or she will guide you on how to prepare yourself for it.
Generally, you’ll be required to make some lifestyle adjustments like quitting smoking (if you’re a smoker), exercising regularly, eating healthy, and stopping certain medications. Such changes are necessary to minimize risks and quicken post-operation recovery.
If you’ve more questions about minimally invasive spine surgery or any other spine-related disorders and treatments, feel free to reach out to us. Also, you can book an appointment to see one of our orthopedic doctors in Dubai.




 Injury to the extremities and trunk is quite common which almost everybody gets by normal activities or by an accident like playing football, lifting heavy weight etc.. There seems to be the confusion about application of ice or hot pack and how long one should use after the injury.
Injury to the extremities and trunk is quite common which almost everybody gets by normal activities or by an accident like playing football, lifting heavy weight etc.. There seems to be the confusion about application of ice or hot pack and how long one should use after the injury.

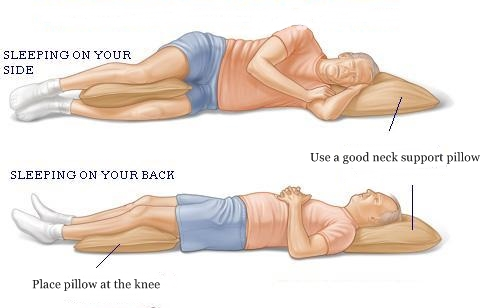
 Recent research reveals that nearly one in three people experience back pain after a night’s sleep, No one really understands the reason for morning stiffness. Presumably, while the body is inactive, fluid leaks out from the small blood vessels and capillaries and the tissues become “waterlogged.” Then, if you try to move the part, the swollen tissues feel stiff until the motion pumps the fluid out through the lymph channels and the veins while most feel stiff or ache.
Recent research reveals that nearly one in three people experience back pain after a night’s sleep, No one really understands the reason for morning stiffness. Presumably, while the body is inactive, fluid leaks out from the small blood vessels and capillaries and the tissues become “waterlogged.” Then, if you try to move the part, the swollen tissues feel stiff until the motion pumps the fluid out through the lymph channels and the veins while most feel stiff or ache.