Symptoms
The most common early symptom of Alzheimer’s is difficulty remembering newly learned information.
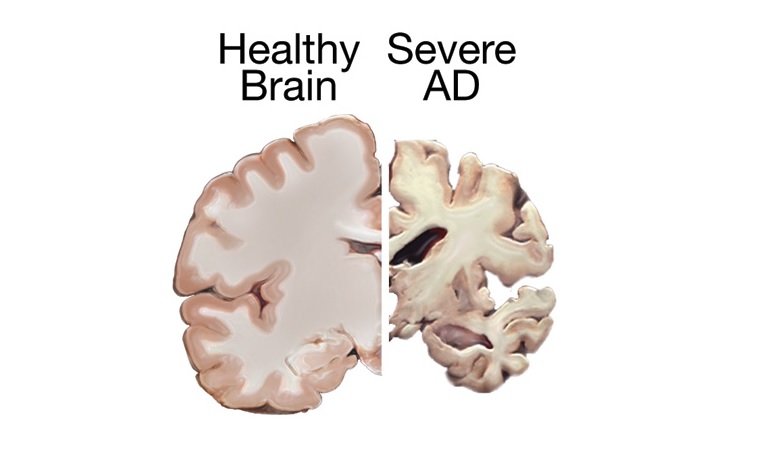
Just like the rest of our bodies, our brains change as we age . Most of us eventually notice some slowed thinking and occasional problems with remembering certain things. However, serious memory loss, confusion and other major changes in the way our minds work may be a sign that brain cells are failing.
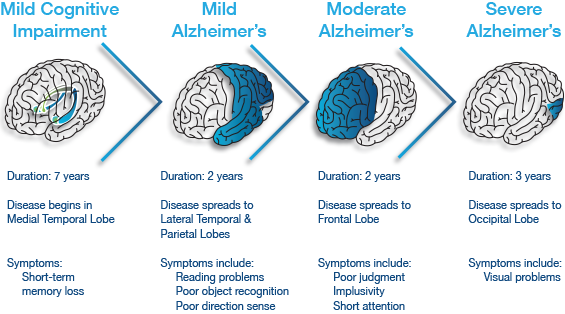
The most common early symptom of Alzheimer’s is difficulty remembering newly learned information because Alzheimer’s changes typically begin in the part of the brain that affects learning. As Alzheimer’s advances through the brain it leads to increasingly severe symptoms, including disorientation, mood and behavior changes; deepening confusion about events, time and place; unfounded suspicions about family, friends and professional caregivers; more serious memory loss and behavior changes; and difficulty speaking, swallowing and walking.

Alzheimer’s is not the only cause of memory loss.
Many people have trouble with memory — this does NOT mean they have Alzheimer’s. There are many different causes of memory loss. If you or a loved one is experiencing symptoms of dementia, it is best to visit a doctor so the cause can be determined.
The role of plaques and tangles
Plaques and tangles tend to spread through the cortex as Alzheimer’s progresses.
Two abnormal structures called plaques and tangles are prime suspects in damaging and killing nerve cells.
Tangles are twisted fibers of another protein called tau (rhymes with “wow”) that build up inside cells.
Though most people develop some plaques and tangles as they age, those with Alzheimer’s tend to develop far more. They also tend to develop them in a predictable pattern, beginning in areas important for memory before spreading to other regions.
Scientists do not know exactly what role plaques and tangles play in Alzheimer’s disease. Most experts believe they somehow play a critical role in blocking communication among nerve cells and disrupting processes that cells need to survive.
It’s the destruction and death of nerve cells that causes memory failure, personality changes, problems carrying out daily activities and other symptoms of Alzheimer’s disease.
Diagnosis of Alzheimer’s Disease
Doctors use several methods and tools to help determine whether a person who is having memory problems has “possible Alzheimer’s dementia” (dementia may be due to another cause) or “probable Alzheimer’s dementia” (no other cause for dementia can be found).
To diagnose Alzheimer’s, doctors may:
- Ask the person and a family member or friend questions about overall health, past medical problems, ability to carry out daily activities, and changes in behavior and personality
- Conduct tests of memory, problem solving, attention, counting, and language
- Carry out standard medical tests, such as blood and urine tests, to identify other possible causes of the problem
- Perform brain scans, such as computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET), to rule out other possible causes for symptoms.
These tests may be repeated to give doctors information about how the person’s memory and other cognitive functions are changing over time.
Alzheimer’s disease can be definitely diagnosed only after death, by linking clinical measures with an examination of brain tissue in an autopsy.
Treatment of Alzheimer’s Disease
Alzheimer’s disease is complex, and it is unlikely that any one drug or other intervention can successfully treat it. Current approaches focus on helping people maintain mental function, manage behavioral symptoms, and slow or delay the symptoms of disease. Researchers hope to develop therapies targeting specific genetic, molecular, and cellular mechanisms so that the actual underlying cause of the disease can be stopped or prevented.


 The World Health Organization estimates that over 800,000 people die by suicide each year – that’s one person every 40 seconds. Up to 25 times as many again make a suicide attempt. There are many, many more people who have been bereaved by suicide or have been close to someone who has tried to take his or her own life. ‘Connect, communicate, care’ is the theme of the 2016 World Suicide Prevention Day. These three words are at the heart of suicide prevention.
The World Health Organization estimates that over 800,000 people die by suicide each year – that’s one person every 40 seconds. Up to 25 times as many again make a suicide attempt. There are many, many more people who have been bereaved by suicide or have been close to someone who has tried to take his or her own life. ‘Connect, communicate, care’ is the theme of the 2016 World Suicide Prevention Day. These three words are at the heart of suicide prevention. Social connectedness reduces the risk of suicide, so being there for someone who has become disconnected can be a life-saving act. Connecting them with formal and informal supports may also help to prevent suicide. Individuals, organisations and communities all have a responsibility here.
Social connectedness reduces the risk of suicide, so being there for someone who has become disconnected can be a life-saving act. Connecting them with formal and informal supports may also help to prevent suicide. Individuals, organisations and communities all have a responsibility here. Open communication is vital if we are to combat suicide. We need to discuss suicide as we would any other public health issue if we are to dispel myths about it and reduce the stigma surrounding it. Equipping people to communicate effectively with those who might be vulnerable to suicide is an important part of any suicide prevention strategy. Showing compassion and empathy, and listening in a non-judgemental way is very important.
Open communication is vital if we are to combat suicide. We need to discuss suicide as we would any other public health issue if we are to dispel myths about it and reduce the stigma surrounding it. Equipping people to communicate effectively with those who might be vulnerable to suicide is an important part of any suicide prevention strategy. Showing compassion and empathy, and listening in a non-judgemental way is very important. All the connecting and communicating in the world will have no effect without care. We need to ensure that we are caring ourselves. We need to look out for others who may be struggling, and let them tell their story in their own way and at their own pace.
All the connecting and communicating in the world will have no effect without care. We need to ensure that we are caring ourselves. We need to look out for others who may be struggling, and let them tell their story in their own way and at their own pace.



 Children are not immune to forces that have driven many adults toward healthy lifestyles and spa and wellness therapies. They too are living in an electronic-gadget-obsessed world, crouching over devices, as they’re fed information and images at incredible speed. Children spend more time than ever hunched over glowing screens.
Children are not immune to forces that have driven many adults toward healthy lifestyles and spa and wellness therapies. They too are living in an electronic-gadget-obsessed world, crouching over devices, as they’re fed information and images at incredible speed. Children spend more time than ever hunched over glowing screens.
 Watch for signals of eye problems– Parents should be alert to symptoms that could indicate an eye or vision problem, such as complaints of eyestrain, headaches and squinting when reading or performing other common activities like regular rubbing of the eye etc. Other symptoms to look for include a white or grayish-white coloring in the pupil, one eye that turns in or out, or eyes that do not track in sync together.
Watch for signals of eye problems– Parents should be alert to symptoms that could indicate an eye or vision problem, such as complaints of eyestrain, headaches and squinting when reading or performing other common activities like regular rubbing of the eye etc. Other symptoms to look for include a white or grayish-white coloring in the pupil, one eye that turns in or out, or eyes that do not track in sync together. For school-age children, a vision screening, which is less comprehensive than a dilated eye examination by an ophthalmologist,can be performed by a pediatrician, family physician, nurse or trained technician during regular checkups. If the screening detects a problem, the child may need to see an ophthalmologist — an eye physician and surgeon.
For school-age children, a vision screening, which is less comprehensive than a dilated eye examination by an ophthalmologist,can be performed by a pediatrician, family physician, nurse or trained technician during regular checkups. If the screening detects a problem, the child may need to see an ophthalmologist — an eye physician and surgeon. Beware of television on hand held devices– It is now becoming more and more common for children to suffer from eye strain after staring at screens for hours and hours. This is sometimes known as computer vision syndrome. Watch out for dry, red and sore eyes. Sometimes, children may experience blurry vision and have problems with words moving on the screen because their eyes are not properly aligned. You can avoid eye problems setting in at an early age by making sure that sessions involving near screen work are limited to 30 minutes a time. Make sure that there are plenty of breaks and that outdoor activity is not neglected.
Beware of television on hand held devices– It is now becoming more and more common for children to suffer from eye strain after staring at screens for hours and hours. This is sometimes known as computer vision syndrome. Watch out for dry, red and sore eyes. Sometimes, children may experience blurry vision and have problems with words moving on the screen because their eyes are not properly aligned. You can avoid eye problems setting in at an early age by making sure that sessions involving near screen work are limited to 30 minutes a time. Make sure that there are plenty of breaks and that outdoor activity is not neglected.